Empowering Patients in Sickle Cell Treatment Approval
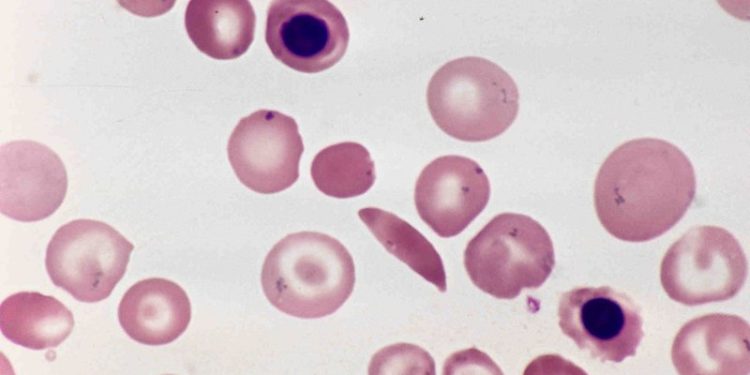
The approval of Casgevy, a new gene therapy for sickle cell disorder, has been a landmark event—not only for its groundbreaking technology but for how it was shaped by the voices of those it seeks to help.
For the first time, the UK’s Medicines and Healthcare products Regulatory Agency (MHRA) involved patients’ experiences as central to the approval process, using their insights to guide assessments.
This pioneering move reflects a profound shift toward patient-centered healthcare, ensuring treatments address the real needs of those affected.
The Importance of Patient Voices in Healthcare
For over 18,000 people in the UK living with sickle cell disorder, the challenges are significant and deeply personal. Sickle cell can affect nearly every aspect of life, from work and relationships to school and social activities.
Patients often experience severe pain episodes, a situation described by John James, CEO of the Sickle Cell Society, as a “huge impact” on daily life. Despite the widespread impact, sickle cell has historically seen limited advancements in treatment options, leaving many patients feeling overlooked.
The MHRA’s decision to involve sickle cell patients in the approval process for Casgevy represented a breakthrough. By integrating the lived experiences of those who know the condition best, the agency was able to gain a fuller understanding of the disorder’s impact and the potential benefits of the treatment.
How Patients Shaped the Casgevy Approval
In collaboration with the Sickle Cell Society, the MHRA worked with three individuals diagnosed with sickle cell, gathering their feedback on quality of life, treatment expectations, and hopes for gene therapies.
These discussions occurred from April to August 2023, during which each participant met with the MHRA’s assessment team to share their perspectives.
One patient expressed the personal significance of being part of the process, saying,
“It was so important to me that the voices of people who live with the condition were heard and understood.” They continued, “Making my contribution to a decision about such a life-changing therapy is really important to me. Seeing it approved gives me hope for the future.”
Such insights provided an irreplaceable depth to the MHRA’s evaluation, offering a human angle that purely clinical data could not capture.
According to Julian Beach, MHRA’s Interim Executive Director of Healthcare Quality and Access,
“The patients involved in the licensing of Casgevy helped us gain a thorough understanding of the impact of sickle cell on the quality of their lives and the significant challenges that come with it.”
What Casgevy Brings to the Table
Casgevy is not just another medication—it’s a gene therapy developed using CRISPR, an advanced tool that enables precise DNA editing.
Potential Benefits of Casgevy for Sickle Cell Patients
| Benefit | Description |
|---|---|
| Long-term Solution | Potentially a one-time treatment, reducing the need for lifelong blood transfusions. |
| Improved Quality of Life | Reduced pain episodes, improved health, and greater physical capability. |
| Economic Impact | Patients may experience fewer sick days, contributing to the workforce. |
| Reduction in NHS Costs | Fewer hospitalizations and emergency visits could lead to reduced healthcare costs. |
As Casgevy gains approval, hopes are high that it will not only relieve the burden on patients but also offer societal benefits, including economic advantages through improved patient productivity.
The Future of Patient-Centric Approvals
The MHRA has signaled that patient involvement in Casgevy’s approval was not a one-off experiment but a new standard they aim to follow more frequently.
According to John James of the Sickle Cell Society,
“The MHRA is clearly an organisation that talks about involving patients, and here is a real example of them doing so.”
By including patients, the MHRA was able to gather insights that reflected the full spectrum of needs within the sickle cell community. This collaboration allowed regulators to understand better not only the physical toll of the disease but also the emotional and psychological impact on patients and their families.
The move has set a precedent, highlighting the value of engaging patients as partners in healthcare decisions.
Approval and Access
With Casgevy’s approval, the next steps involve determining access through the NHS. The National Institute for Health and Care Excellence (NICE) will independently assess Casgevy for use in the NHS, which could bring this transformative treatment to more patients in the UK.
The integration of patient voices in Casgevy’s approval process has shown that when regulators and patients work together, the outcomes can resonate deeply with those affected.
This approach, the MHRA hopes, will become a model for future treatment approvals, ensuring that patients’ perspectives are not just considered but are essential to the evaluation of new treatments.
Sources: THX News & Medicines and Healthcare products Regulatory Agency.