In a groundbreaking study published by the National Institutes of Health (NIH), researchers uncovered how inflammation alters the body’s ability to sense heat and touch.
Conducted by teams at NIH’s National Center for Complementary and Integrative Health and the National Institute of Dental and Craniofacial Research, the research offers a detailed look at the biology behind inflammatory pain.
How and Why the Research Was Conducted
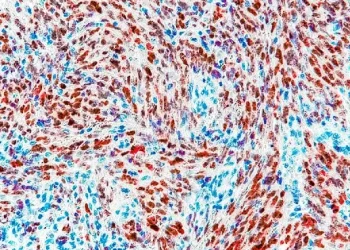
The study, carried out in specialized NIH sensory labs, focused on the molecular behavior of somatosensory neurons—the nerve cells responsible for interpreting physical sensations.
Scientists used advanced imaging and molecular analysis to observe how these cells responded to heat and touch before and after inducing inflammation. The findings are expected to influence future strategies in pain management.
What the Study Found: Distinct Pain Pathways
At the core of the research was the discovery that different neurons respond to gentle touch and intense heat. Under normal conditions, these sensory signals remain separate. But when inflammation is introduced—specifically using prostaglandin E2, a known pain-inducing molecule—key changes occur.
“We saw that neurons responsible for pain became overly responsive to heat, a process that lasted long after the inflammation began,”
explained Dr. Alex Chesler, senior investigator.
Interestingly, the sensation of touch remained unchanged in isolation. However, when combined with inflammatory signals, it became painful—resulting in a condition known as tactile allodynia.
How Inflammation Alters Sensory Response
Effects Observed in Mouse Models
The team used mouse models to closely mimic human neural behavior. Though limitations exist, the neural similarities are significant.
Ongoing Nerve Activity
Chronic inflammation led to prolonged activation of nociceptors—neurons that detect harmful stimuli. This contributed to heightened sensitivity and prolonged discomfort, especially to heat.
Findings at a Glance
| Sensory Feature | Normal Condition | Inflammation Condition |
|---|---|---|
| Heat Sensation | Handled by specific heat neurons | Nociceptors become hypersensitive |
| Gentle Touch | Processed by separate neurons | Unchanged alone, painful with inflammation |
| Overlap in Signals | Minimal | Increased during high-intensity stimuli |
| Tactile Allodynia | Absent | Present when inflammation is active |
Why This Research Matters
This study helps explain why heat feels more painful when inflammation is present, and how otherwise non-painful touch can become unbearable in conditions like arthritis or fibromyalgia.
Key insights include:
-
Pain signals can originate from normal pathways amplified by inflammation.
-
The PIEZO2 ion channel may be central in converting touch into pain.
These findings provide a biological roadmap for developing more precise pain treatments, potentially reducing dependence on broad-spectrum drugs like opioids.
Next Steps in Pain Research
NIH researchers plan to continue exploring how specific cellular receptors and ion channels interact during chronic inflammation. Their aim is to isolate the “switches” responsible for intensifying pain and develop drugs that selectively block these pathways.
-
Targeted therapies may focus on desensitizing overactive nociceptors.
-
Non-opioid pain treatments could benefit from this cellular insight.
The Future of Pain Relief
This NIH discovery marks a turning point in how we understand the body’s pain mechanisms. By distinguishing between normal and inflammation-driven sensory pathways, scientists can now pursue more effective, tailored pain treatments.
Explore more insights from NIH research and follow updates on advances in sensory neuroscience.
Sources: National Institutes of Health.